I'm writing this after the surgery happened because I was far too loopy to write this during recovery. The following events happened on January 17th, 2020.
When we got to the hospital we walked to the surgery center, and shortly after I was called into a back room. My partner, CJ, came with me. The nurse instructed CJ to wipe me down with antibacterial wipes - arms, chest, groin, butt, but not my legs, apparently, because I shaved them within the last two weeks. I used the bathroom real quick, realizing I better not have a full bladder when they administer the anesthetic. When I was done I wrapped up in the hospital gown that so gloriously shows off my butt.
I sat on the table and a nurse came in to put in the IV, and the anesthesiologist came in to say hi and get a couple of my signatures for consent. The nurse giving me the IV actually offered to numb my hand, which was very helpful! That made the whole process a lot more bearable! She did everything with far more expertise than anyone else I've had, and as a fun bonus, she also reminded me of a friend of mine.
After cracking plenty of jokes, because apparently my reaction in these situations is to become hilarious, it came time to wheel me off. I was given what the anesthesiologist called "happy time" medications through my IV. This is where things get fuzzy, and my jokes became very nonsensical... He claimed I wouldn't remember even being wheeled out of the room, and he was mostly correct, except that I do remember the act of being wheeled out, and I remember CJ recording a video.
(I had to upload this one to YouTube because the file size was too big)
As shown in the video, CJ wasn't allowed to follow me into the next room. In that room I think I got onto another table, and the anesthesiologist told me to bend over forward as I sat. I had a couple of pokes at the base of my spine, which caused me to yelp rather more loudly than I expected I would. It didn't hurt that badly, it just was a very strange and somewhat shocking sensation. I remember another nurse saying he's on a roll today, because I guess he administered my anesthetic impressively fast.
I remember nothing else after that except waking up in another bed with very heavy eyelids hearing nurses talking around the room. I tried to open both eyelids, but the double vision was very real, so I closed my left eye in order to at least see what was around me. Keeping even just my right eye open was quite a chore. If I remember correctly, this was the exchange I had with the nurse overseeing my recovery,
"CJ... Huh? Oh, hello."
"Hi, how you doing?"
"I'm coming about. Is CJ here?"
"Not yet, we'll bring you to your family soon."
"Oh good. I want to make sure he knows I'm okay."
As I was laying there, loopy as heck, I overheard some other nurses talking about some personal stuff. One was apparently having a very rough day, and had to deal with some very tough patients. So I spoke loudly enough for them to hear,
"Remember to breathe! You're doing admirable work! I appreciate you, even if your patient doesn't! I hope tomorrow is a better day!"
She replied, "I have tomorrow off, so it will definitely be better."
I said, "Well there you go, treat yourself to something nice!"
The other nurse she was talking to chuckled a bit, and so did my nurse. I recognized how funny this must've been for them, considering I'm crazy loopy and barely awake. My nurse asked why I only had one eye open. I replied,
"Because I can't see straight in 3D, so I have to limit myself to 2D, otherwise everything is double vision. I can open my other eye for you, though, to prove I can."
I opened my left eye and closed my right. She seemed to want both open at once, so I indulged her for a moment, then closed them again saying it was making me motion sick to have both open with double vision.
After a bit of waiting, the double vision gradually got better, and I was wheeled to the waiting area to be reunited with my family. I asked CJ to record a quick video for Facebook, to let everyone know I was okay.
We all went up the elevator to a floor I'd never been to and I was wheeled in to my hospital room. This room was actually quite nice! It had some decent furniture, cool remote controlled lights, and the bathroom was huge.
 |
| Asian Noodle Stir-fry |
I had room service, and the food was surprisingly good. I wish I got pictures of the bathroom, but I did get pictures of the food.
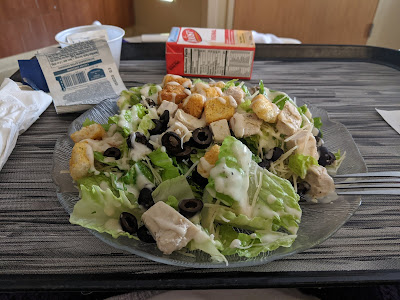 |
| Chicken Caesar Salad |
Unexpectedly, after my delivery to this room, they had me stand up off my portable hospital bed and walk to my new bed. I was not expecting to stand up until at least two days from then, but I guess they wanted to make sure my legs worked, and they wanted to kickstart my body to remind it that I'm alive. They told me I had to walk again later that night after dinner, so I should rest up and prepare for that.
Later that night, with the help of holding onto my IV pole, I managed to walk around the loop of rooms on that floor. I wasn't expecting I could walk that far, but I guess I surprised myself, just as the nurse said I would.
We got back to my hospital bed and I figured out an effective way to sit back down without hurting myself by balancing my thigh against the arm of the bed as leverage. I was pretty tired after that walk. I asked CJ if they would be willing to sleep with me that night so I wasn't alone, and they said yes. As my parents were leaving for the night my dad came over and kissed me on the forehead, which is something I don't think he had done since I was somewhere around 3 or 4 years old. <3
Later that night, with the help of holding onto my IV pole, I managed to walk around the loop of rooms on that floor. I wasn't expecting I could walk that far, but I guess I surprised myself, just as the nurse said I would.
I was awoken every few hours during the night for pain medication and antibiotics, and to drain my catheter bag. After breakfast and lunch, my parents showed up and I did another walk around the loop of rooms. Dr. Stiller came in that afternoon to ask if I felt good enough to head back to my Airbnb. I said yes, as long as it means I get to have my IV taken out. And so my IV was taken out! I went back to my Airbnb that evening with blood bags and a catheter hanging from the wrappings of my abdomen.
And thus begins my recovery! Every 3 hours I alternate in taking 600mg of ibuprofen and 975mg acetaminophen, every 6 hours I take 300mg of gapabentin, and every 12 hours I take 400-80mg of sulfamethoxazole-trimethoprim with a probiotic.
Further updates as events warrant. ;)
